National Referral Hospital, Honiara, Solomon Islands – Team Blog, October 2024
Our recent outreach trip aimed to build upon the foundational work established during our initial 2023 visit to the National Referral Hospital (NRH). This visit focused on deepening collaborations with local orthopaedic surgeons, registrars, nurses and physiotherapists, while also introducing our anaesthetist with expertise in regional anaesthesia to the NRH team. This collaboration is especially timely, given the critical shortage of general anaesthetic medications currently affecting the Solomon Islands. We were also privileged to introduce Dr Craig Buchan, our interventional radiologist, to the NRH radiology department, supporting advancements in the diagnosis and treatment of musculoskeletal conditions using available imaging modalities such as X-ray, CT and ultrasound.
Our team comprised A/Prof David Graham (Orthopaedic Hand Surgeon/Team Leader), Dr Anna Watson (Orthopaedic Hand Surgeon), Dr Tom Matthiesson (Anaesthetist), Dr Craig Buchan (Interventional Musculoskeletal Radiologist), Lynette Sarquis (RN), Kylie Flynn (Hand Therapist) and Cathy Merry (Hand Therapist).
One objective was to foster interdisciplinary collaboration, particularly in patient triage, handover procedures, and treatment planning. Effective coordination between orthopaedic surgeons, physiotherapists, radiologists, and theatre staff is essential to optimise patient outcomes and streamline care.
To bolster surgical capabilities, we provided targeted resources for hand surgery, including:
1. Two refurbished pneumatic tourniquet machines with cuffs,
2. A set of high-quality, adjustable Zeiss surgical loupes,
3. Used orthopaedic instrument sets (Synthes small fragment/ankle set),
4. Various additional supplies.
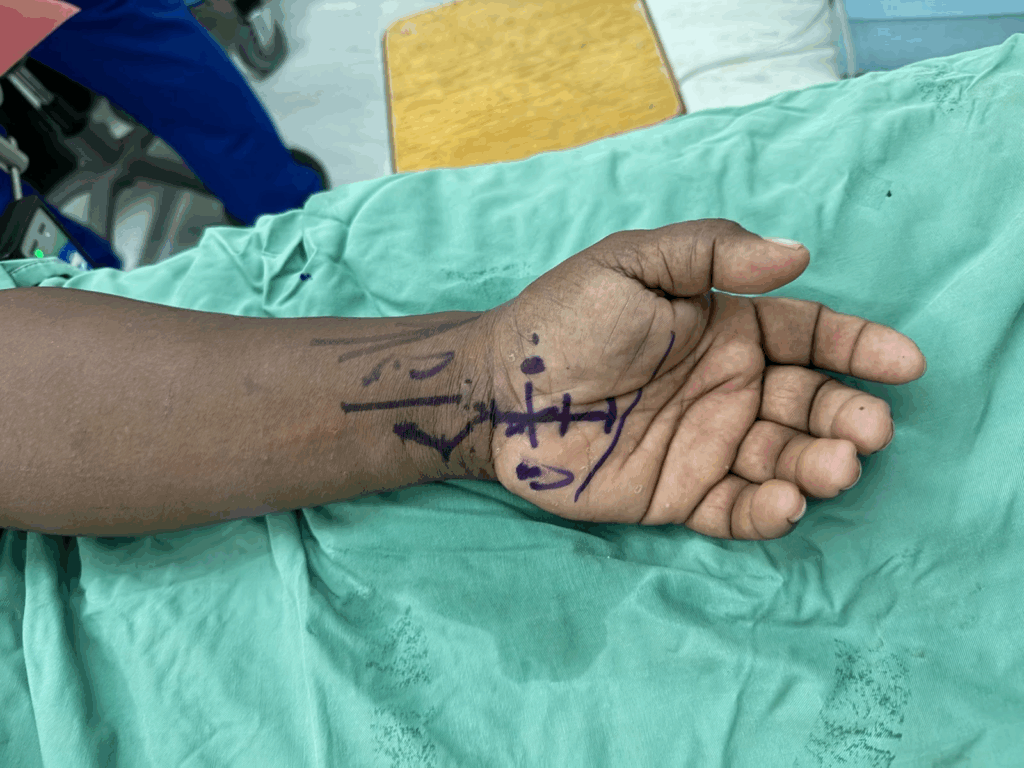
A primary focus on the trip, was on enhancing patient safety protocols. These measures are crucial in promoting safer surgical practices and minimising preventable errors. We reinforced previously implemented strategies, including standardised “time-out” checks, preoperative limb marking, and improved sharps handling with specialised dishes donated for this purpose. Ensuring that each patient’s limb is marked preoperatively and that the “Team Time Out” process is strictly followed was essential. This step includes verifying patient identity with name bands or, when unavailable, using temporary markings, such as on the sole of the foot, and cross-checking the planned procedure with all team members. This protocol serves to bolster patient safety and mitigate the risk of errors.
Diathermy (Monopolar/Bipolar) Best Practices:
• Grounding Pad Placement: Position the grounding pad carefully, avoiding bony areas or locations with metal implants to reduce the risk of burns.
• Power Settings: Utilise the lowest effective power to minimise thermal spread and potential tissue damage.
• Skin Integrity: Regularly check the grounding pad to ensure skin integrity and prevent burns.
• Cables and Connections: Ensure cables remain dry and away from flammable materials, avoiding wet surfaces to maintain safety.
Documentation and Counting Protocols:
Accurate documentation is critical. Emphasising correct count practices prevents surgical items from being inadvertently left inside the patient, which could lead to serious complications, infections, and the need for additional surgeries. Initial, intraoperative, and final counts ensure that all items remain accounted for throughout the procedure.
Tourniquet Management:
• Time Tracking: Record both the application and release times accurately on the patient’s record.
• Regular Updates: Notify the surgeon of elapsed tourniquet time at regular intervals (e.g., every 30 minutes) to maintain awareness.
• Maximum Time Limits: Aim to limit tourniquet time to approximately two hours to minimise risks such as nerve damage and tissue ischemia.
• Documentation: Ensure precise recording of application and release times.
Clinical Support and Instrumentation:
To provide ongoing support, we established regular Zoom meetings to address clinical questions and provide updates. For instrumentation, we transitioned from using single peel packs to organising instruments into two Micro Sets, which allowed for the availability of three complete sets. Additionally, the foam from sterile scrub brushes proved to be a readily available alternative for needle mats, enabling safe sharps handling practices.
Building on previously established relationships, we remain committed to sustaining this partnership through ongoing education, follow-up, and triage discussions. Regular Zoom meetings will continue to serve as a platform for continued learning and case reviews, with sensitivity to cultural and religious factors that have previously influenced participation.
Radiology Notes – Dr Craig Buchan
At NRH (6 Days):
• Collaborated with the Orthopaedic Outreach team on imaging needs and case reviews prior to scheduled surgeries.
• Performed real-time musculoskeletal (MSK) ultrasounds in the Orthopaedic Outpatient setting.
• Promoted stronger communication channels and knowledge sharing between the Orthopaedic and Radiology Departments at NRH.
• Demonstrated the value of a diagnostic/therapeutic MSK ultrasound-guided injection service to support orthopaedic decision-making.
• Provided teaching resources on the indications and applications of musculoskeletal ultrasound.
• Conducted hands-on ultrasound training for radiologists and sonographers, focusing on peripheral joint, tendon, and peripheral nerve imaging.
• Taught basic ultrasound-guided MSK injection techniques to local radiologists, including bursa injections, joint aspiration/injection, ganglion aspiration, and abscess drainage. Reviewed techniques for thoracentesis of pleural effusion and abdominal paracentesis for ascites.
• Reviewed CT practices at NRH using the newly installed Siemens Go.All scanner, supervising radiographer scanning and radiologist reporting for MSK CT cases.
• Introduced the NRH Radiology department to basic CT intervention techniques, covering indications, the consent process, and the roles of nurses and radiographers.
• Taught NRH radiologists basic CT-guided injection techniques, such as joint injections, lumbar nerve root injections, and lumbar facet injections.
• Reviewed oncology CT cases at NRH and coordinated with the Canberra Hospital Medical Oncology Outreach for further support.
At Gizo:
• Assessed the suitability of the Gizo Radiology Department for potential future outreach; it was deemed currently unsuitable.
Educational Sessions:
Orthopaedic Topics:
1. Phalangeal fracture management
2. Metacarpal fracture management
3. Distal radius fracture management
4. Principles of infection and debridement
Radiology Topics:
Formal lectures provided by Dr Buchan included various aspects of musculoskeletal ultrasound and CT-guided intervention.
Formal Lectures Provided by Dr Craig Buchan:
1. Basic Principles of Ultrasound
2. Positioning for Musculoskeletal (MSK) Ultrasound
3. Indications for MSK Injections and Review of Injectables (including Corticosteroids)
4. Imaging Approach to Arthritis
5. Basics of Image-Guided Spinal Injections
6. Assessing Lytic Lesions on X-Ray
Future Education:
Continued education is recommended through monthly Zoom meetings.
Contributions and Donations:
• Dr Buchan, via RAB, provided a Siemens Acuson Portable Ultrasound Machine along with consumables (Tristel Wipes, cleaning supplies, and ultrasound gel).
• Dr Buchan personally donated a textbook on Musculoskeletal Ultrasound (Jacobsen et al).
NRH Radiology Department Resources:
• Three new FujiFilm ultrasound machines donated from Japan. These are modern and highly capable but require additional hockey stick and transvaginal probes. Fuji Applications support is needed to optimize settings for MSK examinations.
• New Siemens Go.All CT scanner in a well-equipped, spacious CT department. Adequate supplies of IV contrast, injectable anaesthetics, and steroids.
NRH Radiology Department Needs:
• A broader range of needles for injections (e.g., 21G in lengths of 30mm, 120mm, and 170mm).
• Larger bore needles for aspiration procedures (e.g., 18G needles of varying lengths).
• CT marking grids.
Observations at Gizo Hospital:
• The digital X-ray machine is currently non-functional.
• The radiology department has a mosquito issue due to a malfunctioning air conditioning system.
• Internet speeds are insufficient for radiographers to download CPD teaching materials.
Reflections on Engagement and Overcoming Challenges in Service Delivery
Initially, there were concerns about engagement and participation, with limited buy-in to Zoom sessions and pre-trip planning. However, after a candid discussion on mutual expectations, we observed a positive shift during this trip, particularly among the local orthopaedic registrars, who demonstrated increased commitment and engagement.
The shortage of general anaesthetic medications presented a significant challenge to service delivery. This issue was mitigated through the judicious use of regional anaesthesia, guided by Dr Tom Matthiesson’s expertise, and the donation of an ultrasound machine. This equipment will allow for the continued practice of regional anaesthesia, providing a sustainable benefit to the NRH team.
Time constraints posed a challenge in balancing surgical duties and teaching. Adding another surgeon to the team next year could enable concurrent surgical and teaching sessions, optimising both service provision and skill development.
Coordinating follow-up care for surgical patients remains a logistical challenge, as many patients return to remote villages or islands, making regular visits to Honiara cost-prohibitive. We are exploring telehealth options and considering regional clinics to improve continuity of care.
On Sunday, some team members ventured to Tenaru Falls for a hike and swim. Despite a punctured tyre and the track closure due to heavy rain, it was a great opportunity for team building and to experience the beauty beyond Honiara.
We would like to extend our sincere gratitude to the Australian Hand Surgery Society and Orthopaedic Outreach for their support through travel grants and much-needed supplies, which made this trip possible.
We would also like to express gratitude to Medartis, KLS Martin and Synthes for loaning and donating equipment.
Overall, we feel this trip was a success, strengthening our ties with NRH and the local team of surgeons, registrars, physiotherapists, anaesthetists, radiologists, and nurses. We look forward to continuing our teaching sessions via Zoom and returning for a follow-up visit in 2025.
Our day trip took an unexpected turn! Tom supervising Clay and Dave changing the tyre.


Cathy providing invaluable post operative hand therapy and educating the local therapists.

The daily ward round.

The beaches outside of Honiara were a great escape.

Kylie and Leanne (local physiotherapist).

Anna, Dave and Craig discussing a case with the local registrars.

Kylie, Lyn and Craig at the physiotherapy department.

The pedicled groin flap was a great case for teaching, and will hopefully provide a durable coverage option for many other patients in the future.

Kylie teaching the local physiotherapists about hand therapy.

Lyn and Joyce (local scrub nurse).

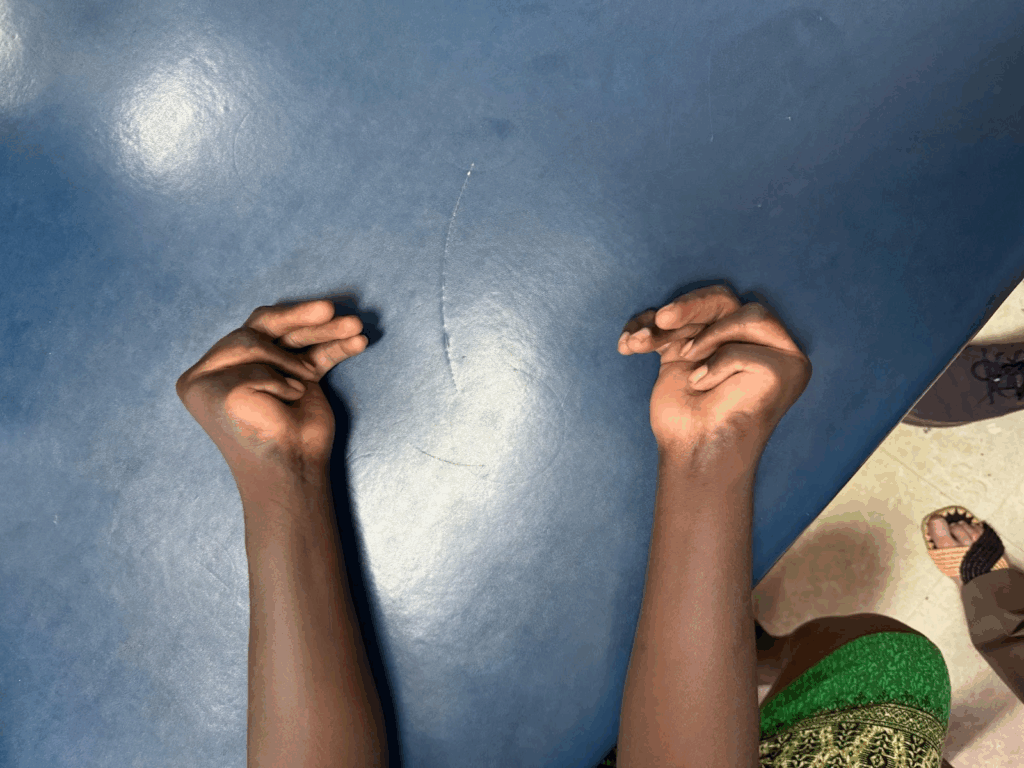
Dave and Anna examining a child and teaching the local registrars on congenital hand deformities.
There was no shortage of interesting hand cases
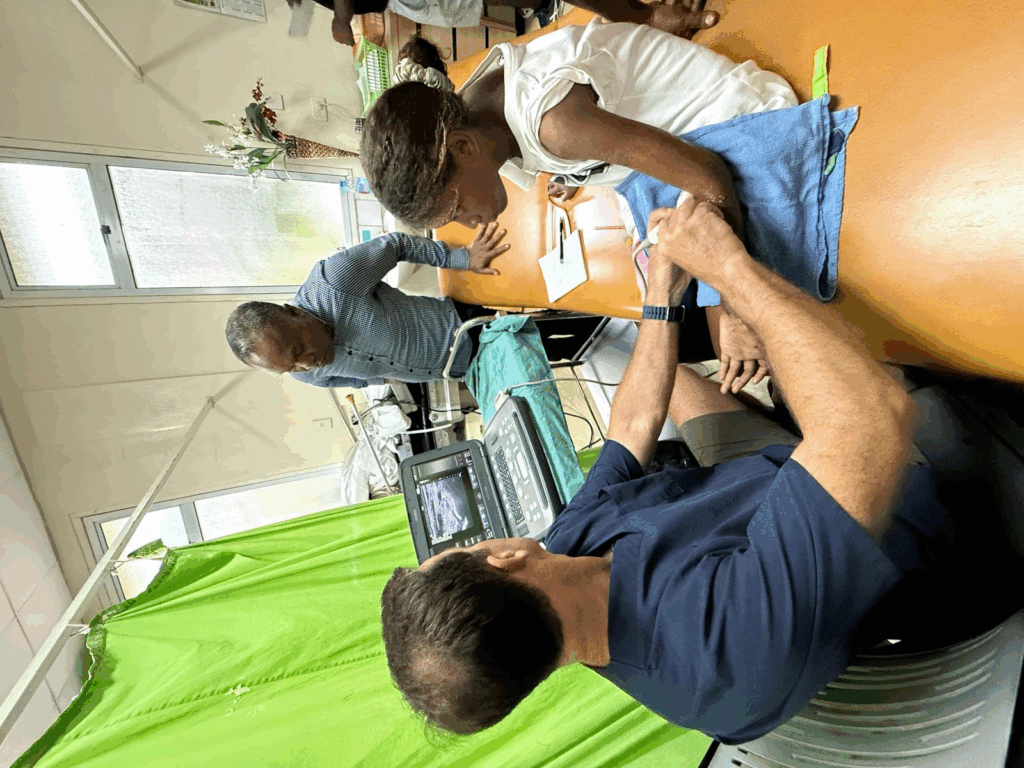
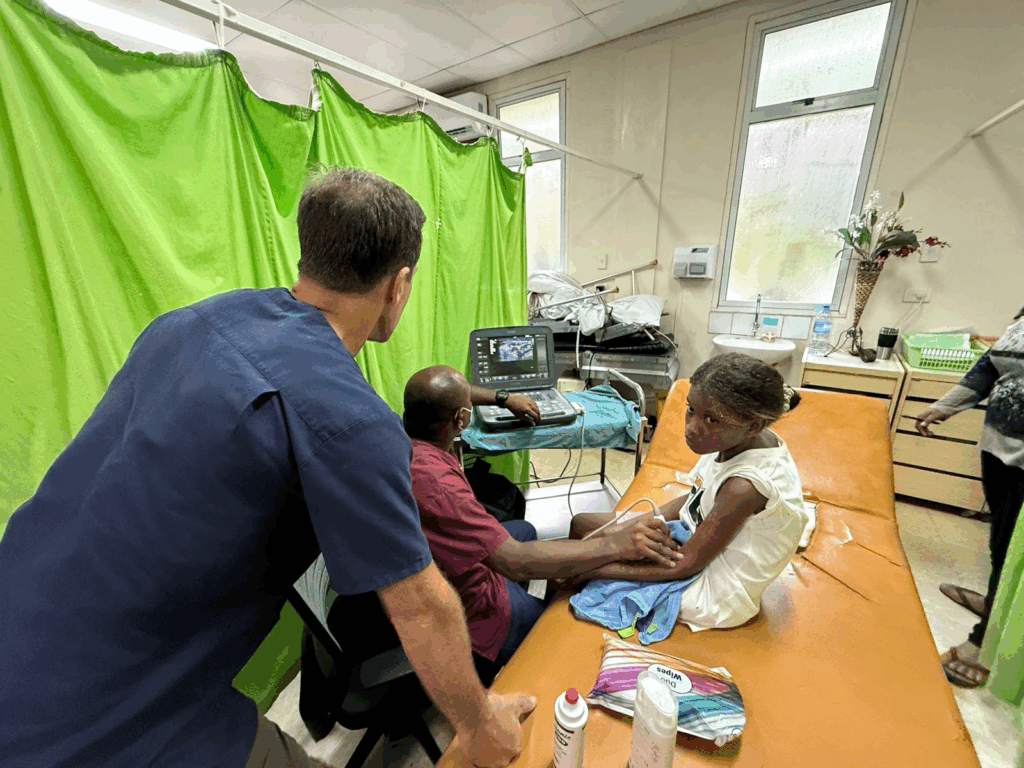
Craig teaching local radiologist (Joseph) on diagnostic ultrasound skills.
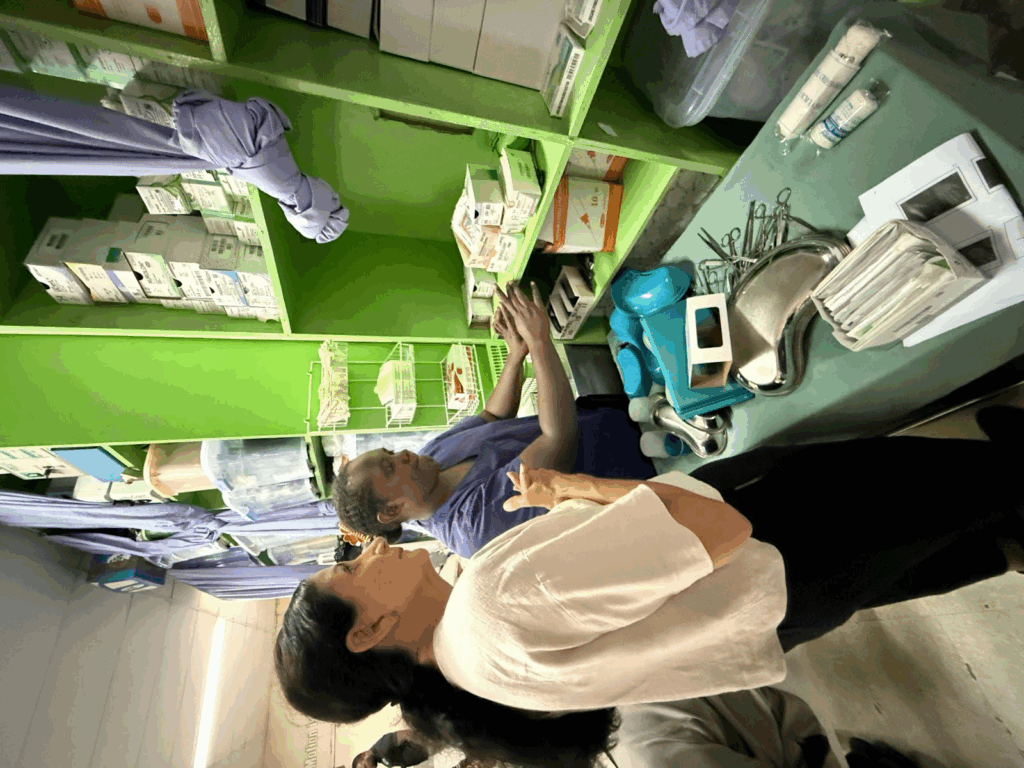
Lyn organising the local equipment to maximize use of available resources, as many supplies were tucked away and not being used.

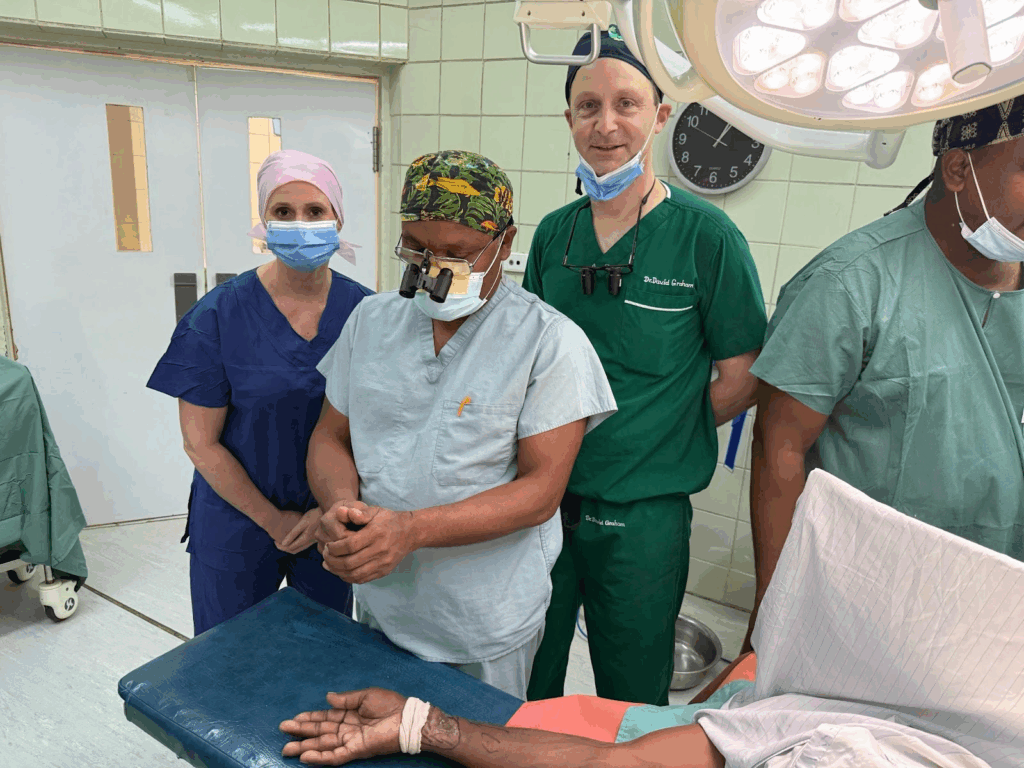
Anna teaching Agnes (local orthopaedic registrar) in theatre.

Craig, Tom and Dave provide support whilst Anna teaches and Lyn assists Joyce (local nurse).
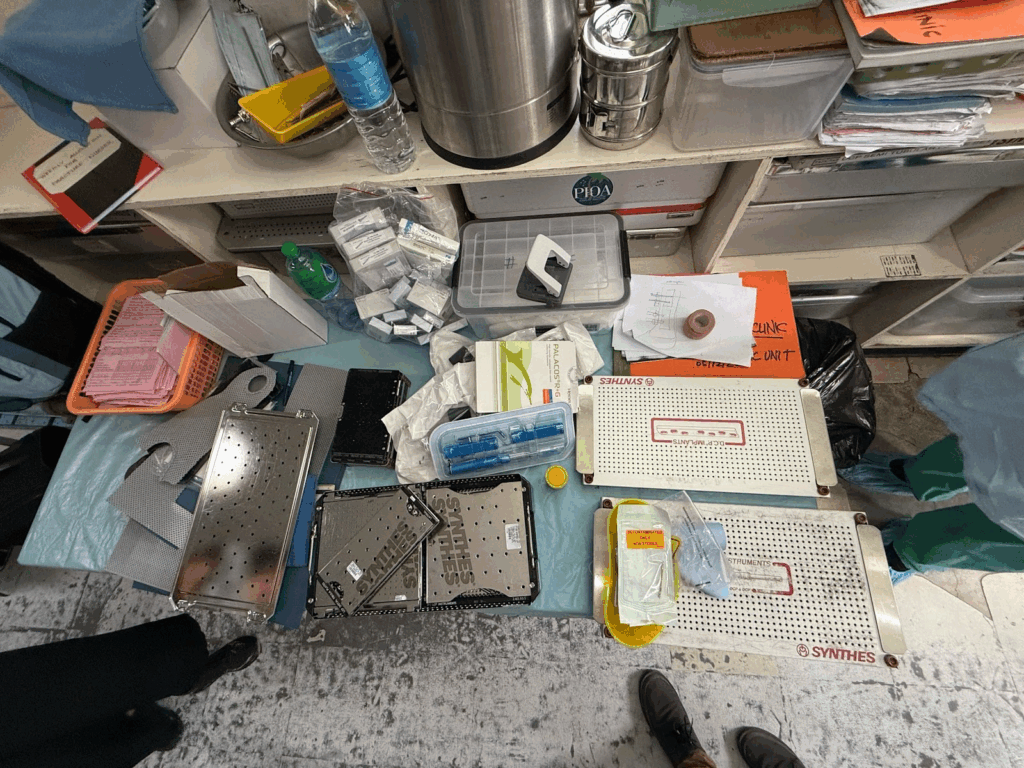
Plenty of donations were gratefully received.
Simple cases provided excellent teaching opportunities.

Anna assisting Oralae (local Orthopaedic registrar) in theatre.
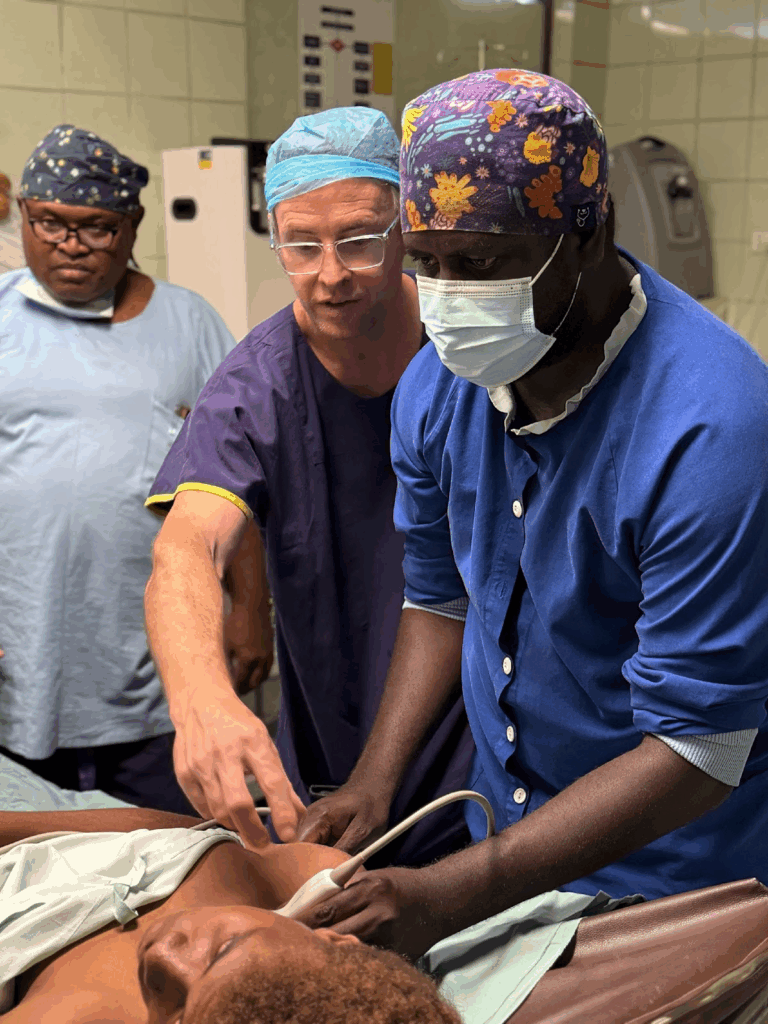
Tom instructing local anaesthetic registrar on regional anaesthetic techniques.

Tom instructing Jack (local anaesthetist) on regional anaesthesia, with the portable ultrasound donated by AHSS.
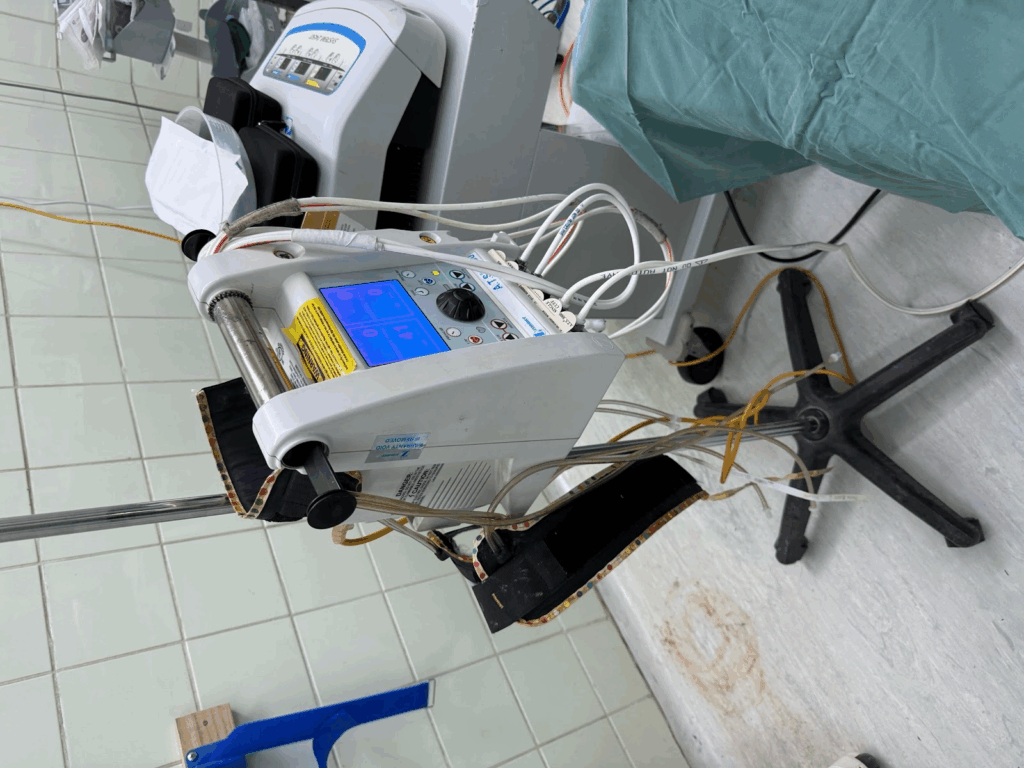
Great to see our donated tourniquets being used, certainly an improvement!

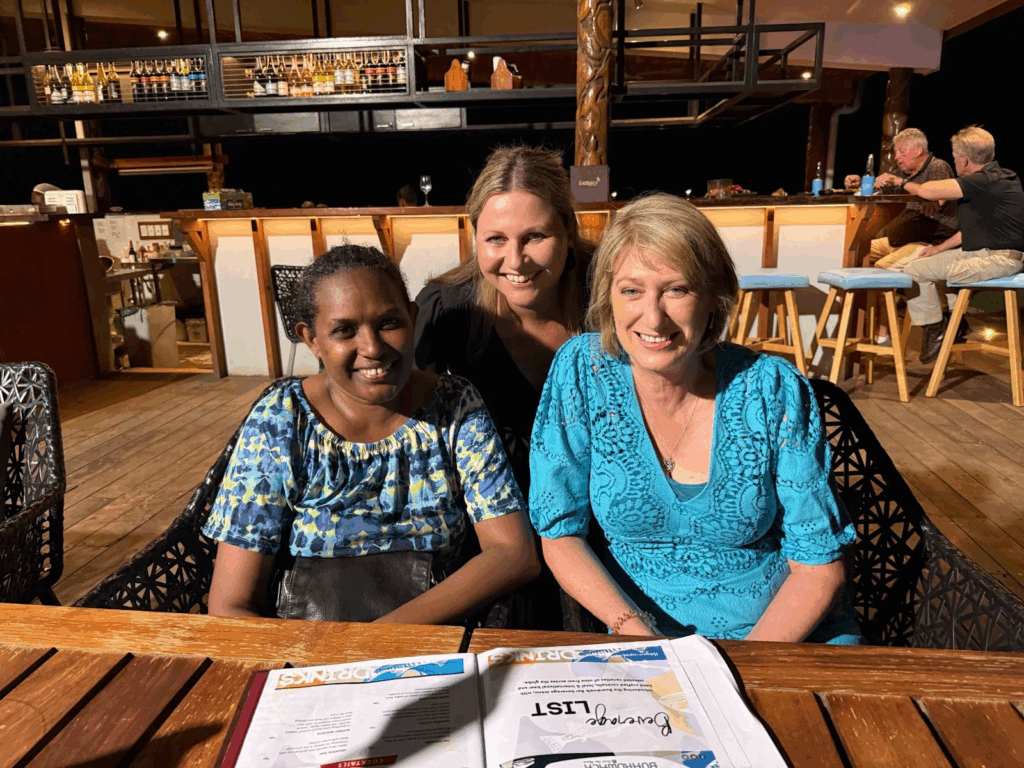
Leanne (local physiotherapist), Kylie and Cathy at the team dinner.

The team thank you dinner.

The team thank you dinner.
Anna, Clay (local orthopaedic registrar/junior consultant) and Dave with the Zeiss loupes donated by the AHSS.




